COVID-19: The Canadian Research Response Panel

Farah Qaiser is a graduate student at the University of Toronto, where she carries out DNA sequencing to better understand complex neurological disorders. When not in the lab, Farah enjoys writing about science and scientists for various media outlets and is one of the co-founders of the Toronto Science Policy Network.
Amid the COVID-19 pandemic, the Canadian government and various funding organizations have invested over one billion dollars into Canada’s COVID-19 research response.
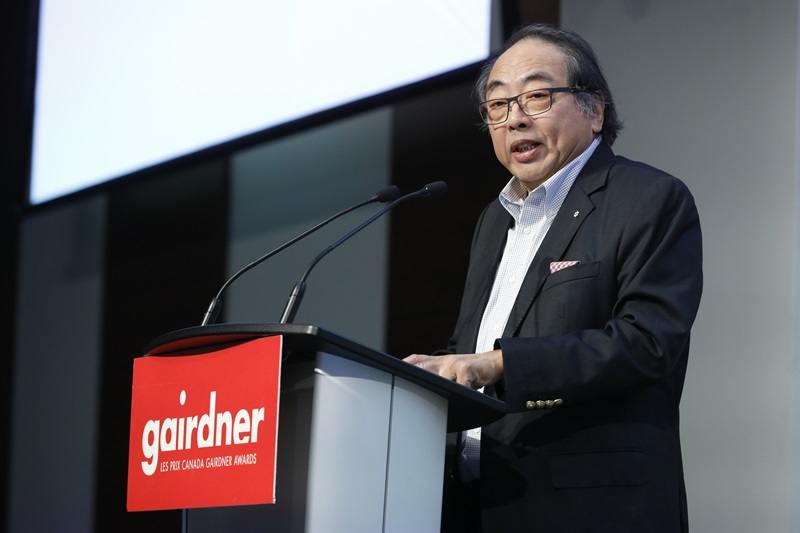
On 29 June 2020, the Gairdner Foundation invited ten leaders to speak about three different aspects of Canada’s scientific response to the pandemic, specifically: vaccine efforts, population-wide research and impact, and co-ordination and collaboration. This panel was moderated by Dr. Janet Rossant, who is the current President and Scientific Director of the Gairdner Foundation.
In her opening remarks, Dr. Mona Nemer, who is Canada’s Chief Science Advisor, thanked the numerous scientists involved in the frontlines of Canada’s research response, including those working in the government, and across industry, non-profit and post-secondary institutions.
“This pandemic has highlighted the role of science and research like never before,” says Nemer, pointing out that it is on us – scientists – to maintain this interest and continue the dialogue.In this post, I’ll highlight some of the key take-aways from this two-hour long panel.
Canadian vaccine efforts
A vaccine helps our body’s immune system to recognize and attack pathogens, such as the SARS-CoV-2 virus which causes COVID-19. As of 29 June 2020, the World Health Organization reported that there are a total of 149 COVID-19 candidate vaccines, where 132 and 17 candidates are in the pre-clinical and clinical stages respectively.

In her talk, Dr. Lakshmi Krishnan, who is the Director General of the National Research Council of Canada’s (NRC) Human Health Therapeutics Research Centre, highlighted how NRC researchers are aiding in vaccine efforts through collaborations and leveraging existing technologies and capacity. This includes a collaboration with VBI Vaccines to develop a vaccine impacting multiple members of the coronavirus family (including COVID-19, SARS and MERS), and working with CanSino Biologics to begin pre-clinical evaluation of their Ad5-nCoV candidate vaccine.

Dr. Volker Gerdts is the Director & CEO of the University of Saskatchewan’s Vaccine and Infectious Disease Organization-International Vaccine Centre (VIDO-InterVac) – which is one of Canada’s largest containment labs. In his talk, Gerdts shared data from VIDO-InterVac’s ferret and hamster models, demonstrating that SARS-CoV-2 replicates in the upper respiratory tract, and that the pathology is consistent with pneumonia. VIDO-InterVac is also currently developing a candidate vaccine, with a proof-of-concept now ready. If all goes to plan, Gerdts hopes that VIDO-InterVac’s vaccine will be ready for the public in the summer of 2021.

Lastly, Dr. Gary Kobinger – a Canada Research Chair in Immunotherapy and Innovative Vaccine Platforms at the Université Laval – walked attendees through his lab’s candidate vaccine, where ongoing challenges include developing animal models and optimizing vaccine delivery. Importantly, Kobinger noted that this candidate is going down the non-profit route – by partnering with GuradRX, he hopes to ensure the vaccine will be available to the entire global community.
Population-wide research and impact
One example of population-wide research can be found in the Canadian COVID Genomics Network (CanCOGeN), which is generating accessible genomics data to inform public health decision-making amid COVID-19. This network was launched by the not-for-profit Genome Canada, in partnership with multiple organizations, including government public health labs, genome sequencing centres, regional Genome Centres and more.

Dr. Rob Annan, who is Genome Canada’s President and CEO, shared that CanCOGeN is undertaking two key genomics projects: (1) to sequence multiple viral samples to better track outbreaks; and (2) to sequence the genomes of patients to better understand why there are such different health outcomes in this disease.
"This is one of the reasons we invest in science in the long-term," says Annan. "This rapid response was really 20 years in the making."
Another example is the COVID Immunity Taskforce, which is leading efforts to implement population-based studies to generate first estimates of SARS-CoV-2 immunity, and investigate the advantages and limitations of immunity testing.

In her talk, taskforce co-chair Dr. Catherine Hankins shared what the group has achieved so far, including determining strategic priorities, establishing an Indigenous Advisory Circle, and launching SeroTracker, which is a dashboard that tracks and synthesizes findings from SARS-CoV-2 serosurveillance efforts worldwide.

To end this session, Dr. Carrie Bourrassa, who is the Scientific Director of the CIHR Institute of Indigenous Peoples’ Health, highlighted the importance of developing culturally safe resources to address COVID-19 concerns among different communities. Here, Bourrassa notes that the OCAP principles are key: ownership, control, access and possession of data. For example, Bourrassa recently partnered with the Canadian Virtual Hospice to develop a culturally safe Grief fact sheet addressing how to process grief during COVID-19.
Coordination and collaboration
With so many diverse research efforts underway, transparency is critical to co-ordinate Canada’s COVID-19 research response.

Dr. Guy Rouleau – who is the Director of the Montreal Neurological Institute and Hospital, and the 2020 Canada Gairdner Wightman Award Laureate – highlighted the role of open science in Canada’s COVID-19 research response. Here, open science refers to scientists being able to freely share data, materials, tools and findings in a timely manner.
“The COVID-19 pandemic has led to an unprecedented adoption of open science in the biomedical field,” said Rouleau, but noted that major lessons are being learned, including the need to implement mechanisms to ensure data quality and rigour in pre-prints, and to change existing institutional policies to favour open science.

Lastly, Dr. Vivek Goel, the Vice-President of Research and Innovation, and Strategic Initiatives, at the University of Toronto, walked attendees through the use of evidence in healthcare, and the different types of decision-making (traditional political decision-making, evidence-based health policy, and evidence-based medicine). "Evidence is always considered within the context of many other factors," says Goel.
Goel also raised an important final point: given that so much money has been invested into Canada's research response, how do we co-ordinate these different efforts effectively? There are some initiatives in progress (such as CanCOVID), but there is a potential for these to become silos too.
The panel ended with closing remarks from Dr. Michael Strong, the President of CIHR-IRSC. Strong remarked that amid of all this turmoil, the importance of science has come to the forefront, especially when it comes to decision-making.
"We need to be very, very careful that we do not let the entire research ecosystem come apart," says Strong, referring to an earlier point raised by Goel - that how we move forward with Canada's entire research ecosystem in these times is also critical.
A visual sketchnote summary of the event. Credit: Farah Qaiser.




-min-(1).tmb-cfthumb_fb.jpg?Culture=en&sfvrsn=ef561fc0_1)

