Gairdner Global Perspectives Panel: COVID-19 – The Road Forward

Farah Qaiser is a graduate student at the University of Toronto, where she carries out DNA sequencing to better understand complex neurological disorders. When not in the lab, Farah enjoys writing about science and scientists for various media outlets and is one of the co-founders of the Toronto Science Policy Network.
On 20 May 2020, the Gairdner Foundation hosted a group of world-renowned experts and Canada Gairdner laureates to explore the science of coronavirus infections. This included important aspects such as the development of new vaccines and treatments, modelling pandemic outbreaks and the implementation of community-led interventions.
This panel was moderated by Dr. Janet Rossant, who is the current President and Scientific Director of the Gairdner Foundation. In this post, I’ll highlight some of the key take-aways from this two-hour long panel.

A visual sketchnote summary of the event. Credit: Farah Qaiser.
Coronavirus infections and the search for antiviral therapies

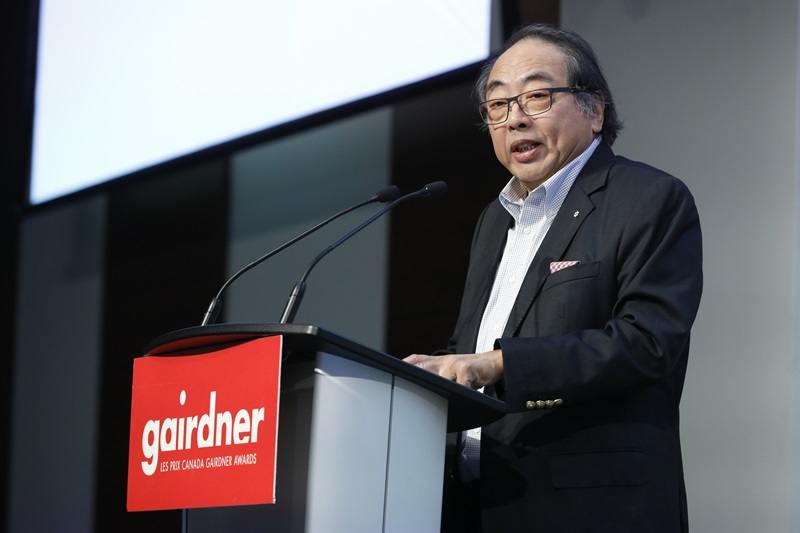
Lorne Tyrrell is the Founding Director of the University of Alberta’s Li Ka Shing Institute of Virology, and a Chair Emeritus at the Gairdner Foundation. He is both a physician and researcher, with significant contributions to hepatitis research and treatment.
In his talk, Tyrrell pointed out that there are three approaches to controlling a new virus: public health measures, antiviral therapies, and vaccines. Here, antiviral therapies refer to drugs which are used to treat viral infections, where potential candidates to treat COVID-19 include Remdesivir. This antiviral was developed by Gilead Sciences to inhibit the Ebola virus, but was instead found to negatively impact zoonotic coronaviruses in general (i.e. a disease that can be transmitted from animals to people). Tyrrell walked attendees through supporting data, where in vitro data suggests that low concentrations of Remdesivir can inhibit SARS-CoV-2, the virus which causes COVID-19, after it enters cells. In addition, Tyrrell shared preliminary results from an NIH clinical trial, which suggests that hospitalized patients with COVID-19 recover 31% faster with Remdesivir than those who did not receive the antiviral.
Tyrrell pointed out that developing antivirals for new viruses take time. For example, the Hepatitis C virus was discovered in 1989, with effective antivirals introduced later in 2014. Importantly, Tyrrell emphasized that waiting for results from “prospective, randomized controlled studies” is critical before introducing any new treatments.
Developing coronavirus vaccines – a worldwide effort

Rino Rappuoli is the Chief Scientist and Head External R&D at GSK Vaccines (Italy), and received a Canada Gairdner International Award (2017) in recognition of his novel vaccine innovation: reverse vaccinology, a genomic approach to vaccine discovery resulting in the life-saving meningococcus B vaccine.
Rappuoli walked attendees through the different types of vaccines that could be developed to treat COVID-19, including RNA vaccines, viral vectors, traditional protein-based vaccines and human monoclonal antibodies. Each vaccine type has its own strengths and advantages. For example, Rappuoli pointed out that RNA vaccines can be produced very rapidly e.g. in 2013, a group of scientists prepared a vaccine against H7N9 influenza to immunise mice in just one week. However, no RNA vaccines have been approved for any diseases yet.
Regardless of what type of vaccine is developed, Rappuoli ended his talk on an important note – that global coordination will be necessary to produce and deliver this COVID-19 vaccine across the world.
Modelling coronavirus outbreaks – when will we know we can lift restrictions?

Christopher Murray is the Director of the Institute for Health Metrics and Evaluation (IHME) and a Professor of Global Health at the University of Washington. He received the 2018 John Dirks Canada Gairdner Global Health Award for quantifying the Global Burden of Disease (i.e. reporting annually on all major diseases by country and year).
Initially, Murray and his team at IHME developed an outbreak model, which takes into account mobility, temperature, testing per capita and population density, to help the University of Washington School of Medicine plan for the first wave of the epidemic. Since then, the model has expanded to include various countries across the world, including Canada. This modelling has also unveiled a few puzzles. For example, Murray notes that in countries like Chile, Argentina and Brazil, despite social distancing and reduced mobility, there are still growing numbers of COVID-19 cases and deaths. In contrast, there are relatively few cases in Pakistan, India and sub-Saharan Africa – have lockdowns worked in these regions?
Moving forward, Murray’s team has many next steps in mind, including extending forecasts to the end of 2020, and introducing projections for sub-Saharan Africa, India (by state), US counties and all low and middle-income countries.
Implementing community interventions in South Africa


Quarraisha and Salim Abdool Karim are the founding leaders of the Centre for the AIDS Program of Research in South Africa (CAPRISA), Professors at Columbia University, and Pro-Vice Chancellors at the University of KwaZulu-Natal in South Africa. They are also the 2020 John Dirks Canada Gairdner Global Health Award laureates for their discovery that antiretrovirals prevent sexual transmission of HIV.
Salim Abdool Karim walked attendees through the COVID-19 situation in South Africa, pointing out that the first case was recorded on 5th March 2020, with a lockdown introduced in late March. The primary goal of this response was to ‘flatten the curve’ i.e. to help health services cope with the COVID-19 case load.
How else did South Africa flatten the curve? Salim Abdool Karim noted that a variety of public health measures that were introduced, including symptom screening, the use of personal protective equipment and increased testing. Importantly, Quarraisha Abdool Karim pointed out that involving local community-based organizations was key in implementing these interventions. With local support, South Africa was able to mobilize the community and have ‘buy-in’ to facilitate home visits, screening and self-quarantine measures.
What brings hope in these uncertain times?
Each panelist cited different reasons for what brings them hope amid COVID-19, ranging from the inspiring level of global collaboration among scientists, the transformation in vaccine development, to how the COVID-19 response has included measures for those disproportionately impacted by the pandemic.
Personally, Murray’s answer resounded with me the most: today, politicians of all stripes are asking for constant input from the scientific community to inform decision-making, and that this prominence of science in everyday discourse offers hope for the future.





.tmb-cfthumb_fb.jpg?Culture=en&sfvrsn=c0e04058_1)



-min-(1).tmb-cfthumb_fb.jpg?Culture=en&sfvrsn=ef561fc0_1)
